Claim analytics

One of the best teams in the country on claims based analytics, we have experience in working with the entire National Claims Data, and additional external data sources to allow our customers take important business decisions using our automated artificial intelligence based analysis. Some of the ways we have helped our clients are as follows
1. Physician Network and Referral Analysis:
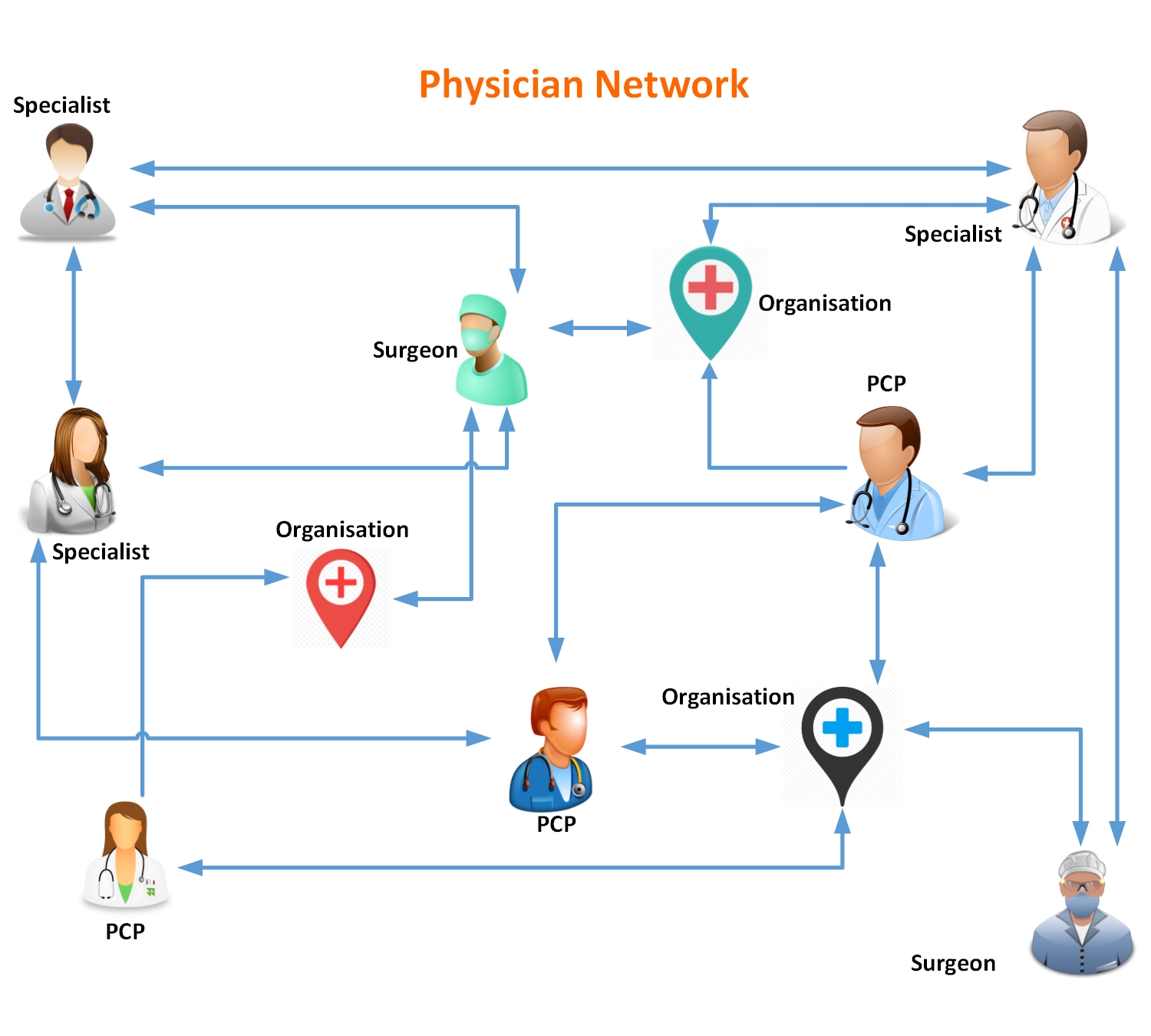
Hospital and ACO management need to understand who are referring to their physicians and what proportion of their clients are being leaked to competitors within their market area. We have developed Loyalty and Volume Score for physicians in the network within the defined market of a client organization and helped identify the most likely physician’s practices that can be acquired to improve business.
2. Entity Resolution:

With increasing volume and velocity of health data, inference across networks and semantic relationships between the health organizations becomes a greater challenge leading to duplicate entities and linkage issue. We use a similarity quotient approach to generate a single entity key by standardizing the organization names and resolving different keys for the same organization using similarities of locations
3. Targeted Campaign for Hospitals:
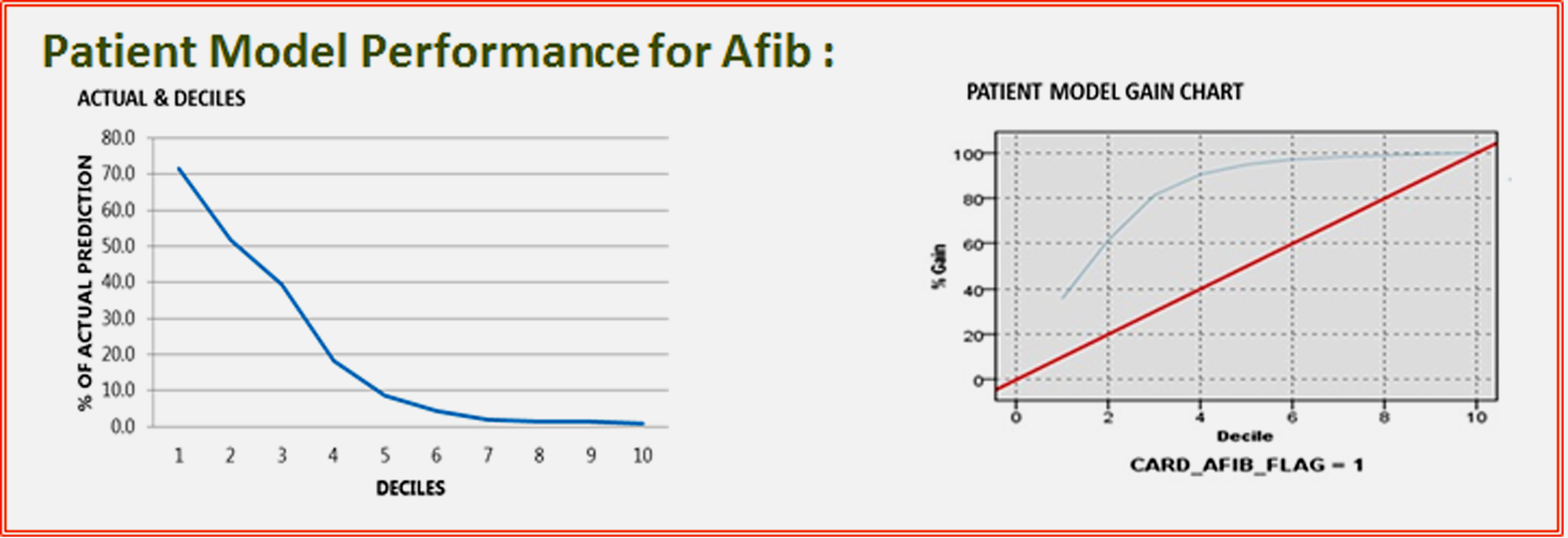
Propensity Models for largest hospital chains in the US to determine prospective consumers for health products related to specific service lines using claims data for patients and survey data for potential consumers in the market area. Models were developed for more than 65 different diseases with patient models having more than 75% response rate and consumer models with greater than 65% success rate.
Telehealth

PROBLEM: Developing an Interactive Alert System through the Case Manager Dashboard to Identify and Respond to Patients Requiring Immediate Attention
Diabetes Patients at a reputed hospital were monitored through the IntelliH Remote Health Monitoring System. Case Managers handling many patients needed to focus on the patients that required immediate attention and an algorithm needed to be formulated to identify such patients with priority levels for this purpose.
SOLUTION: Anytime the patients experienced Blood Glucose excursions and other vital parameters satisfied certain conditions identified by our artificial intelligence based algorithm developed in consultation with their respective Physicians, alerts were sent to the Care Managers so that they could take appropriate action.
BENEFIT: Patients have commented on how timely intervention on the part of their Care Managers helped them avert emergency situations.
Development Environment: Visual Studio 2013, .Net Framework 4.5, Microsoft SQL Server 2008 R2 ; Coding Tools: Asp.Net, C#/VB.Net language, LINQ, Web API. Database: Microsoft SQL Server 2008 R2; External Libraries Used: Clickatell SMS Service, Google GCM (Google Cloud Messaging), .iOS .p12 Certificate